Patients Fear Fallout From NC Medicaid Rate Cuts (reprint)
Image credit: Annabel Podevyn via Unsplash. This is a stock photo and does not represent the individuals mentioned in the article.
By Jaymie Baxley, NC Health News
October 9, 2025
Before he was diagnosed with multiple sclerosis in 2009, Job Gilliam paved roads in the winding mountains of western North Carolina.
Today, the 49-year-old can barely move around his home in rural Catawba County without assistance. His autoimmune disease caused lesions to develop on his spinal cord in 2016, which left him unable to walk.
“It’s got to where I can’t do anything but use a wheelchair, and now I’m kind of bed-bound as well,” he said. “But I’m not going into a facility of any sort, if I can keep out of it. Staying at home is what I’m dead-set on.”
He is able to live on his own because of home care services he receives through Medicaid as part of the state’s Community Alternatives Program for Disabled Adults.
Created for Medicaid beneficiaries who are “medically fragile and at risk for institutionalization,” the program pays for certified nursing assistants who help Gilliam bathe and eat. In general, providing these home care services saves the state money over having someone like Gilliam in a facility.
Nonetheless, an ongoing standoff between the General Assembly and the governor has led the N.C. Department of Health and Human Services to reduce Medicaid reimbursement rates for providers — jeopardizing services that Gilliam and others like him depend on.
“It’s a big concern for me,” he said. “If I’m not going to have CNAs, I’ll have to try to get somebody else to come in their place.”
Missed shifts and last-minute cancellations
Gilliam’s ex-wife died 10 years ago, and none of his four children from that marriage live with him. His girlfriend helps him with basic tasks, but her work schedule prevents her from providing all the daily support he needs.
Gilliam’s only constant companion at home is his dog, Biggie, a 20-month-old Cane Corso named after a legendary rapper.
He’s determined to continue living on his own — a decision that was reinforced in 2020 when he was hospitalized for six months with COVID-19. The experience left him with permanent damage to his lower spine, he said.
The care that allows him to stay at home isn’t always consistent. Lapses in staffing have caused him to go hours and sometimes days without assistance.
Gilliam estimates that he’s been assigned about 25 CNAs in the past six years. He said most of them quit because of low pay.
CNAs earn an average of about $16 an hour in North Carolina. The state’s 80 percent turnover rate for CNAs is among the highest in the nation, according to a 2024 report by the N.C. Health Talent Alliance.
Staffing shortages have led to frequent missed shifts and last-minute cancellations, Gilliam said. He rarely receives the full 50 hours of care he is prescribed each week.
It’s an issue he fears will be exacerbated by the reduced reimbursement rates that went into effect on Oct. 1.
“When you cut the rates, you’re cutting into services for me and other people that need services worse than I do,” he said. “If people ain’t got the money to pay for services on their own, they’re going to have to go into a facility.
“We don’t want to go into facilities. We want to stay home.”
Showdown at the legislature
Lawmakers in Raleigh are deadlocked over Medicaid’s annual “rebase,” the amount of funding needed each year to reflect changes in enrollment, care costs and the rates paid to providers.
In June, the legislature, which has not been able to agree on a full state budget, passed a “mini” budget that targeted specific programs, including Medicaid. But because the mini-budget fell $319 million short of what the state Department of Health and Human Services said it needed for full rebase funding, NC DHHS implemented a series of sweeping cuts to adjust for the shortfall.
Under the announced plan, nearly all Medicaid providers will face rate reductions of 3 percent to 8 percent, while some categories — including nursing homes, hospitals, psychiatric residential treatment facilities and certain ambulatory services — will see steeper cuts of up to 10 percent.
The reductions will affect services across the board, from personal care and home health to outpatient therapy and hospital care.
Provider groups warn these cuts could destabilize health care access in North Carolina — especially in rural and underserved areas. Many smaller hospitals and community-based providers already operate on razor-thin margins, and a 10 percent cut may force them to stop accepting Medicaid patients — or even shutter services entirely.
At the same time, health experts fear the cuts will trigger what Wesley Wallace, a professor of emergency medicine at UNC Chapel Hill, described as a “downward spiral” — less revenue leading to providers who can’t pay staff or maintain services, which leads to further cutbacks or closures.
“If providers are not paid enough to provide care, if hospitals are not provided enough to pay their employees, they will close the doors or dramatically decrease their services,” said Wallace, one of several people who spoke out against the cuts in front of the state legislative building on Sept. 22 while the Senate met inside.
The state’s Republican-led Senate and House of Representatives are not at odds over the rebase itself, which would be fully funded under dueling bills passed by the two chambers in late September.
Their impasse stems instead from a push by the Senate to tie funding for the rebase to an accelerated timetable for lowering taxes, along with a separate allocation of $103 million for the construction of a 500-bed children’s hospital in Apex — both things the House opposes.
In response to the stalemate, Gov. Josh Stein, a Democrat, accused the state legislature of putting politics before people. However, many lawmakers contend that Stein could have instructed NC DHHS, which had money to temporarily cover the shortfall, to delay the cuts.
The department recently floated tapping the state’s Medicaid contingency reserve — a rainy-day fund intended for unexpected costs — as a way to pause or soften the cuts until lawmakers reach agreement. But neither chamber has committed to that route, and the General Assembly is not scheduled to meet again until Oct. 20.
Meanwhile, organizations like the North Carolina Council on Developmental Disabilities have begun soliciting testimonies from people who have been affected by the cuts to share with legislative leaders.
An ‘incredibly uncertain’ future
Chelsea Gray worries the cuts will affect services for Medicaid-covered children with complex needs like her daughter, Molly.
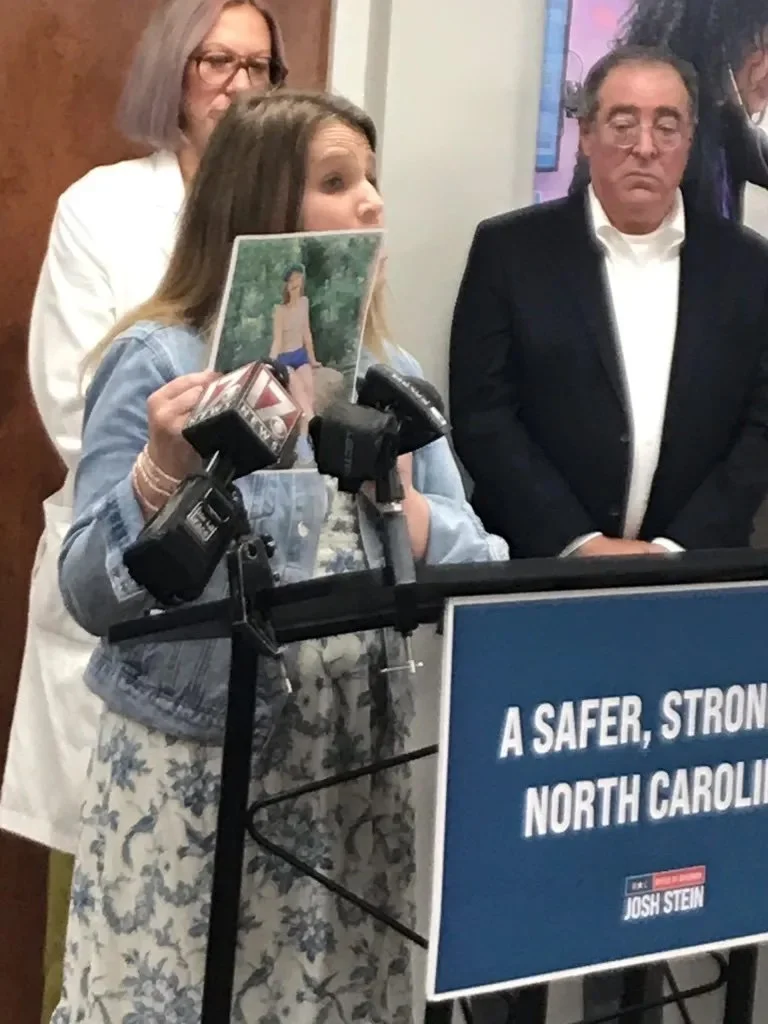
Chelsea Gray of Rutherford County holds up a picture of her daughter during a Sept. 25 news conference. Credit: Anne Blythe / NC Health News
The 14-year-old lives with a medication-resistant, surgery-resistant, non-curable epilepsy, Gray said, causing her to have “around 191 seizures a day.”
Molly’s seizures are tracked through a special medical device, her mother said, and although she has been able to see specialists, the appointments are sometimes four to 11 months out.
Gray shared her concerns with reporters during a recent news conference organized by Stein’s office. She said the cuts could drive some specialists to stop accepting Medicaid, leaving patients with fewer options for care.
“Every single day, we manage unpredictable seizures, navigate limited treatment options with already slammed doctors and face a future that feels incredibly uncertain,” she said. “In a time when it is already difficult to find individuals who are willing to tough this out and do the essential work, I worry about how much more difficult it will be to find care for my child — and all of the children in this state — if Medicaid funding is not protected and provider cuts are put into place.”
Anne Blythe contributed to this report.
This article first appeared on North Carolina Health News and is republished here under a Creative Commons Attribution-NoDerivatives 4.0 International License.![]()
North Carolina Health News is an independent, non-partisan, not-for-profit, statewide news organization dedicated to covering all things health care in North Carolina. Visit NCHN at northcarolinahealthnews.org.
Disclaimer
Individual opinions, findings, conclusions, or recommendations expressed in this content are those of the author(s)/interviewee(s) and do not necessarily reflect the view of the WNC Health Policy Initiative or its host institutions of the University of North Carolina Asheville (UNCA), Mountain Area Health Education Center (MAHEC) or our funders.